Mental Health Initiatives for Underserved Populations: Equity in Care
Understanding Cultural Competence in Healthcare
Culturally competent care in healthcare goes beyond simply acknowledging diversity; it requires a deep understanding and respect for the unique cultural backgrounds, beliefs, and practices of patients. This understanding encompasses not just ethnicity, but also socioeconomic status, religious affiliations, and other factors that shape individual experiences. Effective communication is paramount in achieving cultural competence, meaning actively listening and seeking to understand the patient's perspective. This includes being mindful of potential communication barriers, such as language differences or differing communication styles.
Providers must recognize that their own cultural biases can influence their interactions with patients. Acknowledging and addressing these biases is crucial for delivering equitable and high-quality care. This involves self-reflection and continuous learning about different cultures to foster a genuine appreciation for the diversity within the patient population. This process of self-awareness allows providers to better understand their own limitations and seek appropriate resources to address gaps in their knowledge and understanding.
Addressing the Needs of Diverse Patient Populations
Providing culturally competent care necessitates tailoring treatment plans to the specific needs of each patient. This includes considering factors such as preferred communication methods, dietary restrictions, and traditional healing practices. Understanding these aspects can significantly improve patient engagement and adherence to treatment plans. For instance, respecting a patient's religious beliefs about medical procedures can lead to better cooperation and more positive outcomes.
Furthermore, culturally competent care extends to involving the patient's family and community in the care process, where appropriate. This collaboration can leverage the support systems within the patient's community, leading to a more holistic and personalized approach to treatment. This collaborative approach is especially important in addressing complex health issues that require a multifaceted understanding and intervention.
Implementing Cultural Competence in Practice
Integrating cultural competence into healthcare practice requires a multifaceted approach. This involves developing culturally sensitive policies and procedures, providing culturally appropriate training for healthcare professionals, and ensuring access to interpreters and culturally competent staff. These measures are essential to create a welcoming and inclusive environment for all patients. Creating a system that facilitates communication with diverse patients is critical to building trust and fostering a sense of collaboration.
Beyond the immediate implementation of these practices, it also involves ongoing evaluation and refinement of strategies. Regular feedback from patients and staff is vital for ensuring that efforts to promote cultural competence are effective and meet the evolving needs of the communities served. This continuous feedback loop is key to adapting and improving services to better meet the needs of all patients.
A/B testing, a cornerstone of modern digital marketing and product development, is a powerful method for comparing two versions of something—typically a webpage, an advertisement, or a product feature—to determine which performs better. Essentially, you're presenting two variations (A and B) to different segments of your audience and analyzing which generates the desired outcome more effectively. This might include higher conversion rates, increased engagement, or improved user satisfaction. Understanding the underlying principles of A/B testing is crucial for anyone looking to optimize their online presence and maximize returns.
Expanding Access through Telehealth and Community-Based Initiatives
Improving Access to Mental Health Services
Expanding access to mental health services is crucial for addressing the growing mental health crisis. Telehealth, with its ability to connect individuals with providers regardless of geographical limitations, plays a significant role in increasing accessibility. This is particularly beneficial for those in rural areas or those with mobility challenges, making care more convenient and less intimidating. Community-based initiatives, such as mobile clinics and outreach programs, further extend reach, bringing services directly to underserved populations and fostering a sense of community support.
Addressing Stigma and Promoting Mental Wellness
A significant barrier to accessing mental health services is the pervasive stigma surrounding mental illness. Addressing this stigma through public awareness campaigns, education, and open conversations can destigmatize mental health issues, encouraging individuals to seek help without fear of judgment. This is a crucial component of any comprehensive mental health strategy, fostering a supportive environment where individuals feel comfortable seeking care.
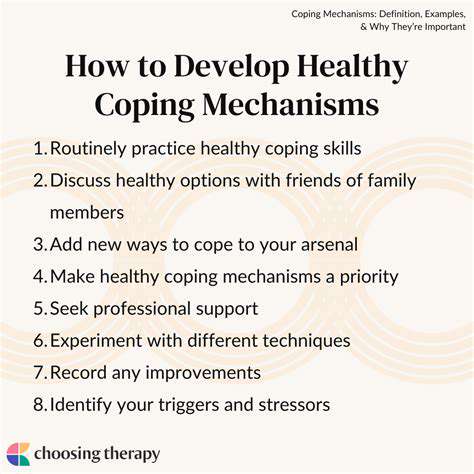
Promoting mental wellness through community programs, workshops, and educational resources can empower individuals to take proactive steps towards maintaining their mental well-being. Encouraging healthy coping mechanisms and stress management techniques empowers individuals to manage their mental health effectively and prevent potential crises.
Telehealth's Role in Expanding Access
Telehealth offers a powerful solution for expanding access to mental health services, particularly in areas with limited provider availability. Virtual appointments allow individuals to connect with therapists, counselors, and psychiatrists remotely, removing geographical barriers and scheduling constraints. This is particularly beneficial for those with busy schedules, mobility issues, or limited transportation options. Telehealth platforms can offer flexible scheduling and convenient access, making it easier for individuals to integrate mental health care into their routines.
Community-Based Initiatives for Outreach
Community-based mental health initiatives are critical for reaching underserved populations. Mobile clinics, outreach programs, and partnerships with community organizations can bring mental health services directly to individuals in their neighborhoods. This approach fosters trust and familiarity, making it easier for individuals to access care in a setting that feels comfortable and supportive. These initiatives are essential in fostering a sense of community ownership and responsibility in mental health.
Addressing Cultural and Linguistic Barriers
Cultural and linguistic barriers can significantly impede access to mental health services. Developing culturally competent mental health providers and offering services in diverse languages are essential steps in ensuring equitable access. This approach ensures that individuals from all backgrounds feel comfortable and respected, promoting trust and understanding in the therapeutic relationship.
Providing culturally sensitive materials and training for providers can help address these barriers. This can include multilingual resources, culturally appropriate therapeutic approaches, and awareness of potential cultural differences in expressing mental health needs.
Collaboration and Partnerships for Enhanced Support
Successful expansion of mental health access requires strong collaboration between various stakeholders. Partnerships with schools, employers, community centers, and healthcare organizations can create a more comprehensive network of support. This approach allows for coordinated efforts to address the mental health needs of the community. Joint initiatives can leverage resources and expertise to develop effective strategies and reach a wider audience.
Sustainability and Long-Term Impact
To ensure the long-term impact of telehealth and community-based initiatives, sustainable funding models and ongoing support are essential. Establishing funding streams that support these programs over time can ensure sustained access to care and prevent a decline in quality or reach. Long-term monitoring and evaluation of the effectiveness of these programs are also crucial to ensuring they continue to meet the evolving needs of the community.
Read more about Mental Health Initiatives for Underserved Populations: Equity in Care
Hot Recommendations
- Customized Sleep Schedules: AI Driven for Sustainable Rest
- Crafting a Personalized Productivity Plan for Mental Clarity
- Sustainable Self Compassion: Cultivating Kindness Towards Your Mind
- Sustainable Productivity Hacks for the Busy Professional
- Sustainable Wellness for Parents: Balancing Family and Self Care
- Data Informed Self Care: Designing Your Personalized Wellness Strategy
- Sustainable Wellness for a Purpose Driven Life
- AI Assisted Mindfulness: Personalized Meditations for Deeper Practice
- Building Inclusive Mental Health Services: Key Initiatives
- AI Powered Self Care: Customizing Your Routine for Maximum Impact