Targeted Therapies for Pet Cancer: Personalized Treatment
The Importance of Genetic Testing in Selecting Targeted Therapies
Understanding the Basics of Genetic Testing
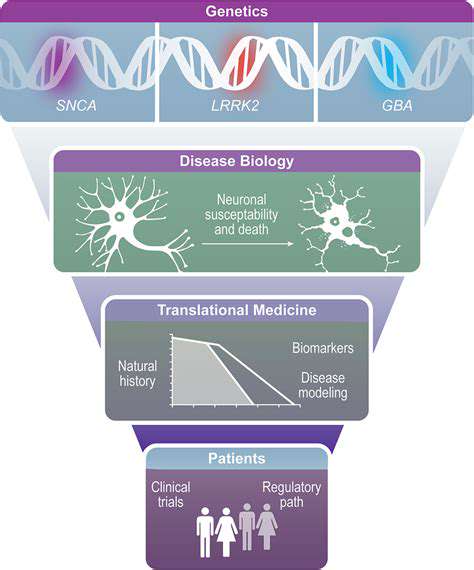
By examining an individual's DNA, genetic testing pinpoints variations that might increase susceptibility to specific diseases. This advanced method offers profound insights into inherited characteristics and possible health vulnerabilities. It's vital to emphasize that genetic test outcomes represent just one component; they must be evaluated alongside a doctor's professional judgment and the patient's comprehensive medical background.
Revealing previously undiagnosed inherited conditions within families is one of genetic testing's most impactful capabilities. For those with a family history of genetic disorders, this knowledge can be transformative. Early identification enables preventive actions like tailored lifestyle changes or specialized monitoring to reduce potential health threats.
Types of Genetic Tests
The landscape of genetic testing includes diverse methodologies, each serving distinct purposes. While some tests focus on individual genes related to particular disorders, others scan wider genomic regions to detect risks for multiple conditions. Selection depends entirely on the individual's specific concerns and ancestral medical patterns.
Particularly valuable are carrier screening tests, which identify whether someone possesses gene mutations that could be inherited by offspring. For prospective parents, these tests provide essential information when considering family planning and assessing risks of genetic conditions in future children.
Benefits of Genetic Testing
Identifying genetic disease predispositions early enables customized prevention strategies and treatment approaches. Such proactive measures frequently result in dramatically better health results and can be life-preserving. Genetic testing's true power lies in equipping people with knowledge to actively shape their health trajectory.
Additionally, these tests inform reproductive choices. Couples gain clarity about potential genetic condition transmission to children, allowing decisions that align with their personal beliefs and family goals.
Accuracy and Limitations of Genetic Testing
While revolutionary, genetic testing has boundaries. Result reliability hinges on both test quality and the analyzing laboratory's proficiency. Selecting accredited facilities and genetics-savvy clinicians is therefore essential.
Proper interpretation requires careful consideration alongside the patient's full medical narrative. Genetic risks don't equate to certain disease development; they merely indicate elevated probability. Environmental influences and lifestyle factors remain crucial health determinants.
Ethical Considerations of Genetic Testing
Genetic testing's implications ripple beyond individuals to affect relatives across generations. Protecting privacy and maintaining confidentiality are critical, necessitating thorough understanding of how results might impact both test-takers and their families.
The Future of Genetic Testing
Continuous technological breakthroughs are expanding genetic testing's precision and applications. Emerging innovations will enable hyper-personalized healthcare strategies, facilitating earlier interventions and more successful treatments for diverse conditions. This evolution will fundamentally transform disease prevention and management paradigms.
Personalized medicine's potential is extraordinary, heralding an era where healthcare adapts to each person's distinctive genetic blueprint.
The Future of Targeted Therapies in Pet Cancer Care
Personalized Medicine Approaches
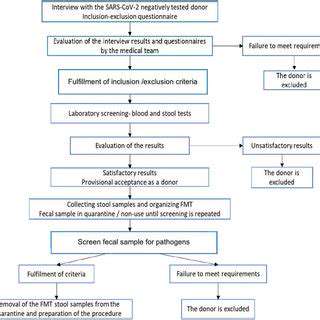
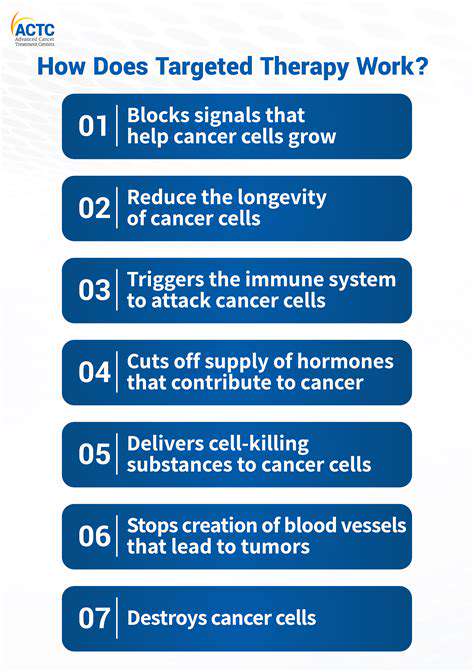
Veterinary oncology is embracing personalized medicine, acknowledging each pet's cancer has unique genetic characteristics. Tumor tissue analysis identifies specific growth-driving mutations, enabling veterinarians to customize treatments that precisely target relevant molecular pathways. This focused strategy enhances effectiveness while reducing adverse effects, representing a significant advancement in pet cancer treatment.
Novel Drug Development and Clinical Trials
Research initiatives continuously develop safer, more potent targeted therapies. Pet-specific clinical trials - collaborations between oncologists, researchers, and owners - evaluate these innovations. These studies generate vital safety and efficacy data, ultimately expanding treatment options for canine and feline cancer patients.
Improving Diagnostics for Early Detection
Enhanced diagnostic tools like molecular testing and advanced imaging enable earlier, more accurate cancer identification in pets. Timely detection typically means more treatment possibilities, better prognoses, and improved quality of life. Such diagnostic progress is revolutionizing veterinary cancer care.
Integrating Targeted Therapies into Existing Protocols
Optimal outcomes require strategic incorporation of targeted therapies with conventional treatments like chemotherapy. This multimodal approach can increase remission rates and survival durations, though implementation requires careful assessment of cancer type and individual pet health factors.
Addressing Resistance Mechanisms
Research focuses on overcoming cancer's adaptive resistance to targeted treatments. Investigational strategies include therapeutic combinations and identification of novel cellular targets, aiming to maintain treatment effectiveness over extended periods and improve long-term survival prospects.
The Role of Immunotherapy in Targeted Therapies
Immunotherapy shows great promise when combined with targeted approaches. By boosting the immune system's cancer-fighting capacity alongside precision treatments, this dual method may significantly enhance therapeutic outcomes. Current research continues exploring these synergistic effects.
The Cost and Accessibility of Targeted Therapies
While cost remains a barrier, initiatives are improving treatment affordability through alternative funding options and cost-reduction strategies. The veterinary community strives to make these advanced therapies accessible to broader populations of pet owners.
Read more about Targeted Therapies for Pet Cancer: Personalized Treatment
Hot Recommendations
- Customized Sleep Schedules: AI Driven for Sustainable Rest
- Crafting a Personalized Productivity Plan for Mental Clarity
- Sustainable Self Compassion: Cultivating Kindness Towards Your Mind
- Sustainable Productivity Hacks for the Busy Professional
- Sustainable Wellness for Parents: Balancing Family and Self Care
- Data Informed Self Care: Designing Your Personalized Wellness Strategy
- Sustainable Wellness for a Purpose Driven Life
- AI Assisted Mindfulness: Personalized Meditations for Deeper Practice
- Building Inclusive Mental Health Services: Key Initiatives
- AI Powered Self Care: Customizing Your Routine for Maximum Impact