The Importance of Hydration in Preventing Urinary Issues
Beyond UTIs: Hydration and Other Urinary Concerns
Understanding Urinary Tract Infections (UTIs)
Urinary tract infections rank among the most frequent bacterial infections, with dehydration being a major contributing factor. The human urinary system relies heavily on adequate fluid intake to function optimally. When insufficient water is consumed, urine becomes concentrated, creating an ideal environment for bacterial growth. Research shows that increasing daily water intake by just 1.5 liters can reduce UTI recurrence by nearly 50%, demonstrating the profound impact of hydration on urinary health.
While UTIs dominate discussions about urinary health, they represent just one facet of a complex system. Bladder function, kidney health, and urinary pH balance all depend on proper hydration levels. The urinary tract's ability to flush toxins and maintain its mucosal lining directly correlates with fluid consumption patterns established over time.
The Role of Hydration in Preventing UTIs
The mechanism by which hydration prevents UTIs involves multiple physiological processes. Dilute urine not only reduces bacterial concentration but also decreases the adherence of pathogens to bladder walls. A study published in JAMA Internal Medicine found that women who increased their water intake experienced 48% fewer UTI episodes than the control group. This protective effect extends beyond simple dilution - proper hydration supports immune cell transport and urinary tract tissue health.
Beyond UTIs: Other Urinary Concerns
Chronic dehydration contributes to various urinary disorders beyond infections. The concentration of minerals in urine increases when fluid intake is low, potentially leading to crystal formation. Over time, these crystals can develop into painful kidney stones. Similarly, inadequate hydration affects bladder muscle function, potentially exacerbating symptoms of overactive bladder and urinary incontinence.
Hydration and Urinary Incontinence
Contrary to popular belief, fluid restriction often worsens rather than improves incontinence. The bladder becomes hypersensitive when chronically dehydrated, leading to more frequent and urgent voiding. Urologists recommend maintaining consistent hydration while addressing incontinence through pelvic floor exercises and behavioral modifications. The ideal approach balances adequate fluid intake with scheduled voiding to retrain bladder function.
Hydration and Kidney Stones
Kidney stone formation follows a predictable pattern when hydration is insufficient. Calcium, oxalate, and uric acid concentrations rise in concentrated urine, reaching saturation points where crystallization occurs. The National Kidney Foundation advises that producing 2-2.5 liters of urine daily can reduce stone recurrence by up to 60%. This requires most adults to consume approximately 3 liters of fluid daily, with water constituting the majority of intake.
Hydration and Overall Urinary Health
The urinary system serves as the body's primary filtration and waste elimination pathway. Every component - from nephrons in the kidneys to the urethral sphincters - functions optimally when properly hydrated. Chronic dehydration forces the kidneys to work harder, potentially leading to long-term damage. Maintaining consistent hydration supports the urinary system's natural detoxification processes and prevents multiple disorders simultaneously.
Choosing the Right Fluids
While water remains the gold standard for hydration, other beverages can contribute to fluid balance when chosen wisely. Herbal teas without caffeine provide hydration along with beneficial phytochemicals. However, drinks containing alcohol, caffeine, or high sugar content can have diuretic effects, potentially counteracting hydration efforts. The American Urological Association suggests limiting coffee and alcohol to 1-2 servings daily for optimal urinary health.
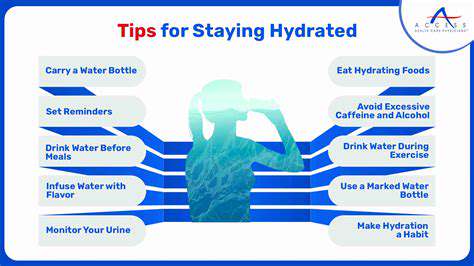
Practical Tips for Staying Hydrated and Preventing Urinary Issues
Understanding Your Hydration Needs
Individual hydration requirements vary significantly based on multiple factors. Body weight, climate conditions, and activity levels all influence fluid needs. A simple calculation suggests consuming 30-35 ml of water per kilogram of body weight daily as a baseline. Those engaging in strenuous activity should add 500-1000 ml per hour of exercise to account for sweat losses.
Monitoring hydration status goes beyond thirst perception. Skin turgor tests, daily weight measurements (1-2% loss indicates dehydration), and urine specific gravity tests provide objective data. Many smartphones now offer hydration tracking apps that incorporate these metrics with personalized reminders.
Incorporating Fluids Throughout Your Day
Modern lifestyles often interfere with natural thirst mechanisms, making scheduled drinking essential. Setting hourly reminders or associating water intake with routine activities (after bathroom breaks, before meals) establishes consistent habits. Glass or stainless steel bottles with measurement markers help track consumption accurately throughout the day.
Enhancing water's appeal can increase voluntary intake. Adding slices of citrus fruits, cucumber, or fresh herbs provides flavor without significant calories. Carbonated water offers an alternative for those who dislike still water's taste. Some find drinking through straws facilitates greater consumption.
The Importance of Recognizing Thirst Cues
Thirst mechanisms become less reliable with age, making proactive hydration strategies crucial for older adults. Dry mouth represents the final stage of thirst - earlier signs include fatigue, headache, and decreased urine output. By the time thirst is perceived, the body may already be 1-2% dehydrated, potentially affecting cognitive and physical performance.
Strategies for Staying Hydrated During Exercise
Athletes require specialized hydration protocols to maintain performance and safety. Pre-hydration (500ml 2 hours before activity) ensures adequate starting fluid levels. During exercise, consuming 150-350ml every 15-20 minutes matches typical sweat rates. For activities lasting over 60 minutes, beverages containing 6-8% carbohydrates and 500-700mg sodium per liter optimize absorption and electrolyte balance.
Post-exercise rehydration should exceed fluid losses by 125-150% to account for ongoing urinary losses. Weighing before and after training provides the most accurate measure of sweat loss - each kilogram lost equals approximately one liter of fluid needing replacement.
Hydration and Overall Health
The systemic benefits of proper hydration extend far beyond urinary function. Every cell in the human body depends on adequate water balance for optimal function. Cerebral spinal fluid production, joint lubrication, temperature regulation, and nutrient transport all require sufficient hydration. Chronic low-grade dehydration has been linked to increased risk of chronic diseases including hypertension and certain cancers.
Emerging research suggests hydration status may influence longevity. A 2023 NIH study found that adults with optimal hydration showed biological aging markers equivalent to being 15 years younger than their chronological age. While more research is needed, these findings underscore water's fundamental role in health maintenance.
Read more about The Importance of Hydration in Preventing Urinary Issues
Hot Recommendations
- Customized Sleep Schedules: AI Driven for Sustainable Rest
- Crafting a Personalized Productivity Plan for Mental Clarity
- Sustainable Self Compassion: Cultivating Kindness Towards Your Mind
- Sustainable Productivity Hacks for the Busy Professional
- Sustainable Wellness for Parents: Balancing Family and Self Care
- Data Informed Self Care: Designing Your Personalized Wellness Strategy
- Sustainable Wellness for a Purpose Driven Life
- AI Assisted Mindfulness: Personalized Meditations for Deeper Practice
- Building Inclusive Mental Health Services: Key Initiatives
- AI Powered Self Care: Customizing Your Routine for Maximum Impact