The Role of Anesthesia in Pet Surgeries: Safety First
Before any surgical procedure, a detailed pre-surgical evaluation serves as the foundation for success and patient safety. This process isn't just about collecting medical records; it's a deep dive into understanding the patient's complete health picture and potential risk factors. Through this comprehensive assessment, surgeons can develop personalized approaches that align with each patient's specific needs.
Identifying possible complications in advance allows medical teams to implement preventive strategies. A thorough evaluation of the patient's physical state helps determine the most suitable surgical method and improves the chances of optimal results.
Assessing Medical History and Current Conditions
The evaluation begins with an exhaustive review of the patient's medical background, including previous surgeries, allergies, chronic conditions, and current medications. Precise documentation enables surgeons to establish a health baseline and spot any existing conditions that might influence the surgery's outcome. This information also proves invaluable when evaluating how the patient might react to anesthesia.
Even minor current health issues can significantly impact surgical procedures. The evaluation must account for these factors to modify the surgical approach and guarantee patient safety.
Identifying Potential Risks and Complications
A key component of pre-surgical evaluation involves recognizing possible risks tied to the planned operation. This requires assessing the patient's overall health, considering age, existing conditions, and lifestyle factors. Anticipating and preparing for potential complications is essential for delivering top-notch patient care.
This risk analysis aids in crafting a detailed surgical plan and implementing preventive actions. Understanding potential risks empowers the surgical team to make well-informed decisions that benefit the patient.
Performing Necessary Diagnostic Tests
Diagnostic testing forms a critical part of the evaluation process. These may include blood tests, imaging studies (such as X-rays, CT scans, or MRIs), and other specialized exams. These tests offer crucial insights into the patient's physical condition and help identify any underlying issues that might affect the surgery.
Test results provide valuable data that guides surgical decisions regarding approach, possible complications, and pre-operative interventions. These assessments ensure patients receive precisely tailored and effective treatment.
Anesthesia Evaluation and Preparation
The pre-surgical evaluation must include a detailed assessment of the patient's suitability for anesthesia. This involves reviewing medical history, current medications, and overall physical condition. Understanding how the patient might respond to anesthesia is vital for minimizing risks and ensuring safety during the procedure.
This evaluation helps determine the appropriate anesthesia type and dosage, contributing to a smooth and secure surgical experience. It's a critical component of pre-surgical care that directly impacts patient well-being.
Patient Education and Consent
An essential part of the evaluation process involves educating patients about their procedure, including potential risks, benefits, and recovery expectations. This empowers patients to make informed decisions and actively participate in their healthcare journey.
Obtaining informed consent is a fundamental requirement. It ensures patients fully understand the procedure's implications and voluntarily agree to undergo surgery.
Selecting Appropriate Anesthetic Agents and Methods
Understanding Anesthetic Agents
Choosing suitable anesthetic agents is paramount for safe and successful procedures. Veterinary anesthesiologists consider multiple factors including patient age, breed, overall health, and the specific surgery being performed. Different agents produce varying effects, and selection aims to minimize risks while maximizing comfort. This involves understanding each agent's onset time, duration, recovery profile, and potential side effects for individual patients.
Available options include inhalant agents like isoflurane and sevoflurane (known for quick action) and intravenous agents like propofol (offering precise control). The selection process weighs potential adverse reactions against the benefits for each specific case.
Evaluating Anesthetic Techniques
Anesthetic methods significantly influence procedure safety and smoothness. Techniques vary based on surgery complexity, patient size, age, and required monitoring level. Intravenous methods allow exact control over anesthesia depth, crucial for managing potential complications. Continuous monitoring of vital signs remains essential throughout the procedure for prompt issue identification.
Modern approaches may incorporate regional anesthesia (targeted nerve blocks), potentially reducing general anesthesia needs and speeding recovery. The chosen technique should align with both patient needs and procedural requirements.
Monitoring During Anesthesia
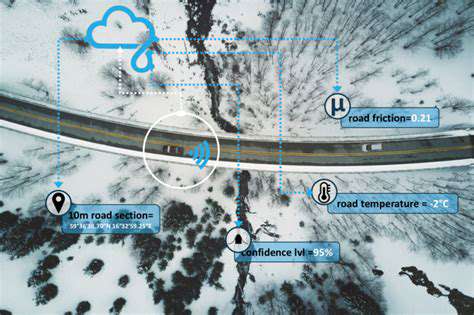
Continuous monitoring forms the backbone of safe anesthetic practice. Veterinary professionals track vital signs including heart rate, respiration, blood pressure, and oxygen saturation to ensure patient safety. These metrics provide real-time feedback about patient response to anesthesia and overall status during the procedure.
Advanced monitoring equipment enables immediate detection of physiological changes, allowing timely adjustments to anesthesia levels or intervention if needed. This continuous oversight helps maintain patient stability throughout the surgical process.
Patient-Specific Considerations
Each patient's unique characteristics influence anesthetic choices. Factors like age, breed, and pre-existing conditions can significantly impact agent selection and technique. Elderly patients, for instance, may require modified approaches due to potential age-related health changes.
Pre-anesthetic assessments including medical history review, physical examination, and possibly bloodwork help customize the anesthetic plan. These evaluations identify potential complications and allow for preventive measures.
Post-Anesthesia Care
Post-operative care is equally critical as the procedure itself. Careful monitoring during recovery ensures smooth transition to normal function. This includes watching for complications like breathing difficulties or temperature regulation issues, and providing appropriate supportive care including fluids and pain management.
Creating a safe recovery environment with continuous monitoring helps address any emerging issues promptly. Understanding the individual patient's response to anesthesia is key to ensuring a comfortable and speedy recovery.
Intraoperative Monitoring: Ensuring Continuous Safety
Pre-Procedure Monitoring
Pre-procedure monitoring establishes baseline physiological data that serves as a reference throughout the surgical process. Recording vital signs (heart rate, respiration, blood pressure) and observing patient demeanor helps identify potential health concerns that might affect anesthesia. Assessing hydration status through physical examination (checking mucous membranes, skin elasticity) informs decisions about fluid therapy needs.
Intra-Procedure Monitoring
Continuous monitoring during anesthesia is essential for patient safety. Tracking vital signs (including ECG readings) provides real-time feedback about anesthetic effects. Blood pressure and oxygen saturation monitoring helps detect potential complications like hypotension or inadequate oxygenation. Observing patient responses (consciousness level, signs of discomfort) allows for immediate adjustments when needed.
Post-Procedure Monitoring
Post-operative monitoring focuses on ensuring smooth recovery. Tracking vital signs, consciousness level, and watching for pain indicators helps assess recovery progress. Special attention is given to respiratory function and potential bleeding, with prompt intervention if any issues arise. This careful oversight contributes significantly to successful patient outcomes.