Internal Parasites in Pets: Detection and Treatment
Effective Treatment Strategies for Internal Parasites

Comprehensive Assessment and Diagnosis
A crucial first step in effectively treating any health concern is a thorough assessment and accurate diagnosis. This involves gathering detailed patient history, conducting physical examinations, and potentially ordering relevant diagnostic tests. A precise diagnosis is essential for tailoring the treatment plan to the specific needs of the individual. A comprehensive evaluation considers all contributing factors, including lifestyle, medical history, and potential environmental influences. This comprehensive approach ensures that the treatment plan is not just addressing the immediate symptoms but also the root causes of the problem.
The diagnostic process should involve collaboration between the patient and healthcare professionals. Open communication and active participation from the patient are vital for obtaining a complete picture of the condition. This collaborative approach allows for a more accurate diagnosis and a more effective treatment strategy tailored to the individual's unique circumstances. Accurate diagnosis is paramount to achieving the best possible outcomes and minimizing the potential for adverse effects.
Pharmacological Interventions
Medication plays a significant role in many treatment strategies. The selection of medications should be based on the specific diagnosis and the individual patient's needs and health status. It is essential to carefully consider potential side effects and interactions with other medications. A thorough review of the patient's medical history is crucial to ensure the safety and efficacy of any prescribed medications.
Pharmacotherapy often involves careful monitoring of the patient's response to treatment. Adjustments to medication dosages or types may be necessary based on observed effects and potential adverse reactions. Regular follow-up appointments are essential to assess treatment efficacy and address any concerns or complications that may arise. Medication adherence is critical for successful treatment outcomes and should be actively encouraged and supported.
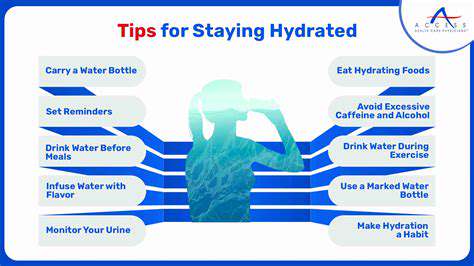
Non-Pharmacological Approaches
Non-pharmacological interventions, such as lifestyle modifications and behavioral therapies, often play a vital role in managing and treating various health conditions. These strategies can include dietary changes, exercise programs, stress management techniques, and relaxation exercises. Implementing these strategies can lead to significant improvements in overall health and well-being. Non-pharmacological approaches often have long-term benefits and can help patients develop healthy habits that promote recovery and prevent future health problems.
Behavioral therapies, like cognitive-behavioral therapy (CBT), can be instrumental in addressing underlying psychological factors that contribute to the condition. These therapies empower patients to develop coping mechanisms and strategies to manage symptoms and improve their quality of life. Individualized programs are essential for tailoring the non-pharmacological approach to the specific needs of each patient.
Supportive Care and Therapies
Supportive care plays a crucial role in providing comfort and improving the overall quality of life for patients undergoing treatment. This can involve various therapies, including physical therapy, occupational therapy, and speech therapy, depending on the specific needs and condition. These therapies aim to enhance physical function, improve independence, and address any limitations that may arise due to the illness or treatment. Supportive care extends beyond medical treatment, focusing on the holistic well-being of the individual.
Addressing the emotional and psychological aspects of the condition is also crucial. This may involve counseling, support groups, or other forms of emotional support. Providing a supportive environment can significantly reduce stress and anxiety, promoting a positive healing experience and improving patient outcomes. Psychological support is essential for patients and their families as they navigate the treatment process.
Monitoring and Evaluation
Regular monitoring and evaluation are essential components of any effective treatment strategy. This involves tracking the patient's response to treatment, identifying any adverse effects, and making necessary adjustments to the treatment plan. Careful monitoring allows for early detection of complications and ensures that the treatment remains effective and safe. Regular assessments help gauge the progress of the treatment and ensure that the chosen interventions are yielding the desired outcomes.
The monitoring process also involves evaluating the patient's overall well-being, including physical, emotional, and social aspects. This holistic approach ensures that the treatment is addressing not only the immediate concerns but also the broader impact on the patient's life. By continuously monitoring and evaluating, healthcare professionals can ensure that the treatment plan remains appropriate and effective throughout the entire process.
Read more about Internal Parasites in Pets: Detection and Treatment
Hot Recommendations
- Customized Sleep Schedules: AI Driven for Sustainable Rest
- Crafting a Personalized Productivity Plan for Mental Clarity
- Sustainable Self Compassion: Cultivating Kindness Towards Your Mind
- Sustainable Productivity Hacks for the Busy Professional
- Sustainable Wellness for Parents: Balancing Family and Self Care
- Data Informed Self Care: Designing Your Personalized Wellness Strategy
- Sustainable Wellness for a Purpose Driven Life
- AI Assisted Mindfulness: Personalized Meditations for Deeper Practice
- Building Inclusive Mental Health Services: Key Initiatives
- AI Powered Self Care: Customizing Your Routine for Maximum Impact